Step 3 – NBME 7 – Block 2
Quiz Summary
0 of 50 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 50 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42
- 43
- 44
- 45
- 46
- 47
- 48
- 49
- 50
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 50
1. Question
A 2-year-old African American girl with sickle cell disease is transferred to the emergency department from a local urgent care center because of a 1-day history of decreased activity, lethargy, and mild periumbilical abdominal pain. She has not had fever, vomiting, or diarrhea. Medical history is otherwise unremarkable. Vaccinations are up-to-date. The child is 85 cm (2 ft 9 in; 25th percentile) tall and weighs 10.5 kg (23 lb; 10th percentile). Vital signs are temperature 37.2°C (99.0°F), pulse 140/min, respirations 20/min, and blood pressure 110/60 mm Hg sitting. The child appears tired and quiet. Results of a complete blood count obtained at the urgent care center are shown:
Blood
Hematocrit
18%
Hemoglobin
6.2 g/dL
WBC
12,000/mm3
Platelet count
85,000/mm3
The remainder of the physical examination is most likely to show which of the following?
CorrectIncorrect -
Question 2 of 50
2. Question
Physicians in the obstetrics and gynecology department at a large medical clinic implement use of a new screening test for ovarian cancer. Three-hundred women with a strong family history for breast and ovarian malignancies undergo the screening test. Positive test results are confirmed with ovarian biopsy. Sixty participants are found to have ovarian cancer. Data analysis shows that the screening test has a 95% sensitivity, a 95% specificity, and an 82% positive predictive value for the diagnosis of ovarian cancer. Based on these results, the physicians plan to provide the screening test for all female patients. Administering the test to all women who come to the clinic is most likely to have which of the following effects on the accuracy of the test?
CorrectIncorrect -
Question 3 of 50
3. Question
A 44-year-old woman comes to the office because of a 4-month history of low mood, insomnia, decreased energy, and loss of interest in her usual activities. She also has had an increased appetite resulting in a 4.5-kg (10-lb) weight gain during this time. She had episodes of major depressive disorder at the ages of 22 and 31 years and believes this could be her third depressive episode. Although she responded well to a selective serotonin reuptake inhibitor after her last episode, she discontinued the medication 10 years ago because of its adverse effects. She has no other history of serious illness and currently takes no medications. She is well groomed and fully oriented. BMI is 26 kg/m2. Vital signs are normal. Physical examination shows no abnormalities. On mental status examination, she is tearful. There is mild psychomotor retardation and poor eye contact. She asks, “Why did this happen again? I’ve been trying so hard not to be depressed, but here I am again.” After expressing empathy, which of the following is the most appropriate physician response?
CorrectIncorrect -
Question 4 of 50
4. Question
A 54-year-old man comes to the office because of a 4-week history of shortness of breath and increasingly severe leg swelling. He had one episode of syncope 1 week ago associated with loss of vision in his left eye. He states that he becomes short of breath after walking more than one block. He has to prop himself up on several pillows at night to avoid a sensation of drowning. Medical history is remarkable for a myocardial infarction 2 years ago treated with a single drug-eluting stent and aspirin and clopidogrel therapy. He was nonadherent to his medication regimen and stopped taking the drug after his prescription ran out. A few days after he ran out of his medication, he developed severe, crushing chest pain but did not seek treatment. Today, vital signs are pulse 92/min, respirations 18/min, and blood pressure 126/84 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 94%. Fine, basilar crackles are heard; there are no carotid bruits. Cardiac examination shows a displaced apical impulse. There is bilateral, pitting pedal edema. A myocardial perfusion scan demonstrates a fixed filling defect with nonviable myocardium involving at least 50% of the left ventricle. Transthoracic echocardiography shows that the affected portion of the myocardium is thinned with paradoxical systolic movement. In addition to prominent Kerley B lines, which of the following findings is most likely to be seen on chest x-ray in this patient?
CorrectIncorrect -
Question 5 of 50
5. Question
A 34-year-old man comes to the office because he and his wife have been unable to conceive for 2 years. Previous evaluation of his wife showed no abnormalities. Medical history is unremarkable, and the patient takes no medications. BMI is 23 kg/m2. Vital signs are within normal limits. Physical examination shows normal-sized testes that are descended. The remainder of the examination shows no abnormalities. Results of serum studies are shown:
Follicle-stimulating hormone
3.0 mIU/mL (N=1.6–8.0)
Luteinizing hormone
5.8 mIU/mL (N=1.5–9.3)
Testosterone, total
615 nmol/L (N=270–1070)
Antisperm antibodies
positive
Further analysis shows that antisperm antibodies are directed against antigens exposed during the acrosome reaction. Semen analysis and genetic testing show no abnormalities. These antisperm antibodies are most likely directed toward which of the following locations in this patient’s sperm?
CorrectIncorrect -
Question 6 of 50
6. Question
A 17-year-old primigravid woman at 12 weeks’ gestation comes to the clinic for her first prenatal visit. Medical history is remarkable for bipolar disorder treated with lithium carbonate. Since beginning lithium carbonate 3 years ago, she has not had any recurrent episodes of mood disorder. Vital signs are within normal limits. Physical examination shows a uterus consistent in size with a 12-week gestation. In addition to starting the patient on a prenatal vitamin, which of the following is the most appropriate next step in pharmacotherapy?
CorrectIncorrect -
Question 7 of 50
7. Question
The following vignette applies to the next 2 items.
A 52-year-old African American man comes to the office for evaluation of diabetes mellitus. He has had diabetes for 11 years for which he has taken glyburide for the past 6 years. He also takes one 81-mg aspirin tablet daily. He recently moved to your area to become the principal of the local high school. His most recent health evaluation was 6 months ago and included a physical examination, laboratory testing, and an ophthalmologic examination. One of his concerns today is that, before moving, his previous physician discussed adding a new medication to “protect” his kidneys. At today’s visit, vital signs are pulse 72/min, respirations 18/min, and blood pressure 124/78 mm Hg. Physical examination, including funduscopic examination, shows no abnormalities. The patient reports mild numbness in his toes. Results of laboratory studies obtained 6 months ago are shown:
Serum
Urine
Creatinine
0.9 mg/dL
Urinalysis
Normal
Glucose, fasting
130 mg/dL
Microalbumin
Normal
Blood
Hemoglobin A1c
6.5%
You recall an article assessing the benefits of an angiotensin-converting enzyme (ACE) inhibitor in normotensive patients with type 2 diabetes mellitus. This was a randomized, double-blind, placebo-controlled study of 156 patients with type 2 diabetes mellitus without microalbuminuria. Patients were assigned to the ACE inhibitor or placebo group and were monitored for 6 years. Results of the study are shown:
Outcome After 6 Years of Treatment With ACE Inhibitor or Placebo
Microalbuminuria
Creatinine
Change in Blood
Change
(% of Patients)
Clearance (mL/sec)
Pressure (mm Hg)
in Hemoglobin A1c (%)
ACE inhibitor
6.5
0.04
−2.7
−0.2
Placebo
19
0.025
−3.2
+0.5
P-value
0.042
0.040
>0.2
0.052
Item 1 of 2
Based on this study, the most appropriate conclusion is that to prevent the development of microalbuminuria in one patient, the number of patients who would need to be treated with an ACE inhibitor is which of the following?
CorrectIncorrect -
Question 8 of 50
8. Question
Item 2 of 2
Based on this study, the most appropriate advice to the patient regarding treatment with an ACE inhibitor is that the therapy will do which of the following?
CorrectIncorrect -
Question 9 of 50
9. Question
An 81-year-old woman comes to the office because of a 1-year history of gradually progressive shortness of breath that is increasingly severe with activity. She has not had chest pain, palpitations, cough, fatigue, nausea, vomiting, or abdominal pain during this period. Medical history is remarkable for hypertension, hypercholesterolemia, and latent tuberculosis. She also has a history of mild to moderate thoracic back pain that is well controlled with acetaminophen. Other current medications include amlodipine, isoniazid, and pravastatin. She had smoked one-half pack of cigarettes daily for 30 years until she quit 35 years ago. She does not drink alcoholic beverages or use illicit drugs. BMI is 26 kg/m2. Vital signs are temperature 37.0°C (98.6°F), pulse 96/min, respirations 16/min, and blood pressure 110/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 94%. Physical examination discloses clear lungs with symmetric chest expansion. There is 1+ pitting edema of the lower extremities up to the knee. A lateral chest x-ray is shown. Which of the following is the most likely mechanism of the findings in this patient?
CorrectIncorrect -
Question 10 of 50
10. Question
A 36-year-old man with a history of alcohol use disorder has been receiving care in the intensive care unit since admission 2 days ago for severe pancreatitis. Physical examination at that time disclosed epigastric tenderness and no other abnormalities. The patient was intubated and mechanical ventilation was subsequently initiated. Medical history otherwise is unremarkable and he takes no routine medications. Since admission, he has been receiving 0.9% saline, propofol, fentanyl, meropenem, and a multivitamin. Temperature is 38.2°C (100.8°F), pulse is 124/min, respirations are 20/min on an Fio2 of 0.60, and blood pressure is 112/64 mm Hg. Pulse oximetry shows an oxygen saturation of 94%. Results of laboratory studies are shown:
Serum
Blood
Lipase
1840 U/L (N<200)
Hematocrit
30%
Calcium
8.8 mg/dL
Hemoglobin
9.8 g/dL
Na+
144 mEq/L
WBC
18,000/mm3
K+
3.4 mEq/L
Cl−
104 mEq/L
HCO3−
20 mEq/L
Protein
Albumin
2.8 g/dL
The patient has been receiving nothing by mouth. Regarding this patient’s nutrition, which of the following is the most appropriate management at this time?
CorrectIncorrect -
Question 11 of 50
11. Question
A 10-year-old girl has long-standing allergic rhinitis, asthma, and sinusitis. She is brought to the office because she has now developed migraine headaches without aura. Which of the following medications is contraindicated in the continued treatment of this patient?
CorrectIncorrect -
Question 12 of 50
12. Question
A 59-year-old woman is admitted to the hospital for evaluation of a 2-day history of worsening dyspnea. She reports shortness of breath when climbing more than five stairs and three-pillow orthopnea. She has not had chest pain. Medical history is remarkable for hypertension, chronic obstructive pulmonary disease, chronic venous stasis with recurrent cellulitis, and anemia of chronic disease. Medications include hydrochlorothiazide, lisinopril, and ipratropium. She smoked one pack of cigarettes daily for 40 years but quit smoking 3 years ago. She is 160 cm (5 ft 3 in) tall and weighs 74 kg (163 lb); BMI is 29 kg/m2. Vital signs on admission are temperature 37.0°C (98.6°F), pulse 96/min and regular, respirations 18/min, and blood pressure 182/98 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 92%. Auscultation of the lungs discloses crackles in the lower half of both posterior lung fields and diffusely decreased breath sounds. Cardiac examination discloses a grade 2/6 early-peaking systolic murmur heard best along the left sternal border that decreases on Valsalva maneuver. There is an S4 gallop. Examination of the lower extremities shows hyperpigmentation of the skin extending to the knees and 1+ edema, bilaterally. Chest x-ray shows new, increased interstitial markings in the upper lung fields. ECG shows sinus rhythm. Intravenous furosemide is administered and the patient’s symptoms improve. One day after admission to the hospital, echocardiogram shows moderate left ventricular hypertrophy but good systolic function. Heart valves are poorly visualized. Which of the following is the most likely explanation for this patient’s symptoms?
CorrectIncorrect -
Question 13 of 50
13. Question
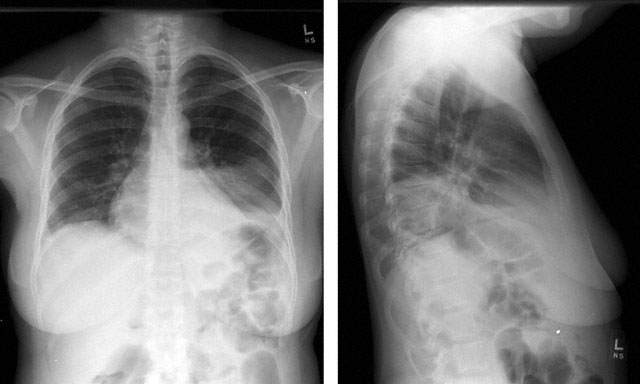
A 76-year-old woman comes to the emergency department because of a 3-day history of worsening shortness of breath. She also reports the onset of a cough productive of blood-tinged sputum and a temperature of 39.1°C (102.4°F) yesterday. Medical history is significant for hypertension, for which she takes losartan. She has no medication allergies. The patient has smoked one-half pack of cigarettes daily for the past 45 years. She is awake and alert but says she feels anxious. BMI is 23 kg/m2. Vital signs are temperature 38.8°C (101.8°F), pulse 112/min, respirations 26/min, and blood pressure 104/78 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 94%. Auscultation of the lungs discloses crackles in the left lung base. Heart sounds are normal. The remainder of the physical examination discloses no abnormalities. PA and lateral chest x-rays are shown. Which of the following is the most significant factor for the increased risk for death in this patient?
CorrectIncorrect -
Question 14 of 50
14. Question
A 62-year-old man comes to the office for a follow-up examination 1 week after undergoing excision and resection of a pigmented lesion on his left cheek that was suspected to be melanoma. Pathology results of the lesion show basal cell carcinoma; however, the margins are not clear and the physician will need to perform another procedure involving wider excision and possible skin grafting. Which of the following is the most appropriate physician statement?
CorrectIncorrect -
Question 15 of 50
15. Question
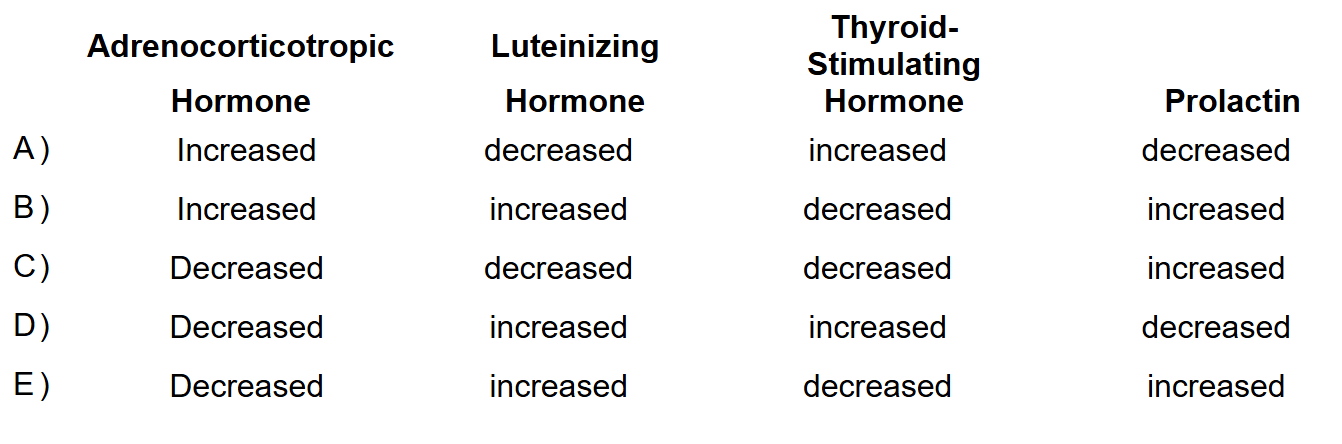
A 55-year-old man comes to the office because of a 3-month history of double vision, headache, and erectile dysfunction. He also has had frequent urination and increased thirst during this time. He has not had fever or pain on urination. He has no history of serious illness and takes no medications. Vital signs are within normal limits. Examination shows no abnormalities. MRI of the brain shows a calcified mass on the sella turcica. Which of the following sets of laboratory findings is most likely in this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 16 of 50
16. Question
A 3-year-old boy is brought to the emergency department by his parents 1 hour after he tripped and fell onto the edge of a coffee table, sustaining a laceration on his forehead. On arrival, he is placed on a cardiac monitor in preparation for conscious sedation. Medical history is unremarkable. Family history is remarkable for hypertension and type 2 diabetes mellitus in his grandfather. The patient’s vital signs are temperature 36.9°C (98.4°F), pulse 83/min, respirations 18/min, and blood pressure 89/62 mm Hg. The patient appears well. Physical examination discloses a 2-cm laceration on the forehead. Lungs are clear to auscultation. Cardiac examination discloses a normal S1 and S2 and no murmur. His heart rate becomes faster during inspiration and slower during expiration. Rhythm strip is shown. The patient’s condition is most likely caused by which of the following mechanisms?
CorrectIncorrect -
Question 17 of 50
17. Question
A 32-year-old woman comes to the clinic for an initial visit because of a 6-month history of progressively worsening episodes of anxiety. The first episode occurred while she was walking home from work and consisted of a feeling of nervousness, shortness of breath, sweating, palpitations, and a fear of falling in the middle of the street and getting hit by a car. After a second similar episode, the patient began to avoid buses and trains. One attempt she made to get on a bus resulted in a severe attack. She continues to leave her house but she will not allow herself to participate in social events that involve travel or more than one other person. She stays away from crowded stores. During the examination the patient speaks rapidly and appears intensely anxious. She has not had suicidal ideation but is preoccupied with thoughts of hopelessness. Medical history is significant for a 7-year history of alcohol use disorder; she stopped drinking 1 year ago and she regularly attended 12-step program meetings until the anxiety began. She was prescribed alprazolam twice daily by her primary care physician 6 weeks ago. The patient says she increased the alprazolam to three times daily because the anxiety persisted. She says, “The medicine doesn’t prevent me from getting anxious but it lowers my anxiety when it comes.” Family history is significant for major depressive disorder in her mother. The patient’s vital signs are normal and physical examination discloses no abnormalities. Which of the following is the most appropriate change to this patient’s medication regimen?
CorrectIncorrect -
Question 18 of 50
18. Question
The medical director of four primary care clinics is concerned about the increasing national incidence of advanced chronic kidney disease among adult patients who have type 1 diabetes mellitus and hypertension. He reviews the clinics’ electronic medical records and identifies 75 adult men and women with stage 2 chronic kidney disease who also have type 1 diabetes mellitus and median systolic blood pressures greater than 140 mm Hg. Only 40% of these patients receive annual measurement of urine microalbumin concentration and only 50% receive ACE inhibitor or angiotensin-receptor blocking agent therapy. The medical director proposes that the practice implement a policy requiring that physicians caring for patients who have chronic kidney disease plus hypertension or type 1 diabetes mellitus receive an electronic alert reminding them to order an annual measurement of urine microalbumin concentration and to prescribe ACE inhibitor or angiotensin-receptor blocking agent therapy. Which of the following best describes the type of intervention proposed by the medical director?
CorrectIncorrect -
Question 19 of 50
19. Question
A 72-year-old woman comes to the office because of fatigue and recent weight loss. She says she has also noticed an increased frequency of bowel movements. She is still active in her church group. Medical history is significant for essential hypertension for the past 20 years that had been well controlled with hydrochlorothiazide. Recently, her blood pressure has been in the range of 150/85 mm Hg to 160/90 mm Hg. Pulse is 104/min and irregularly irregular. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 20 of 50
20. Question
A 78-year-old white woman comes to the office because of a 2-month history of progressively worsening intermittent abdominal pain. She rates the pain as an 8 on a 10-point scale. During the past week it has occurred daily, often after meals. She has no urinary symptoms and has not had a fever. Acetaminophen has not provided relief from the pain. She has had loose stools but has not noticed any blood in the stool. Colonoscopy done 3 years ago disclosed no abnormalities. Medical history is also significant for hypertension and degenerative joint disease affecting both knees. Medications include hydrochlorothiazide and 81-mg aspirin daily. She has lost 7 kg (15 lb) in the past 2 months. She is 160 cm (5 ft 3 in) tall and now weighs 54 kg (118 lb); BMI is 21 kg/m2. Vital signs are temperature 37.2°C (99.0°F), pulse 72/min, respirations 18/min, and blood pressure 126/72 mm Hg. Auscultation of the chest discloses no abnormalities. Abdominal examination discloses slightly decreased bowel sounds but otherwise discloses no abnormalities. Rectal examination discloses soft stool in the rectal vault that is positive for occult blood. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 21 of 50
21. Question
A 65-year-old woman who was diagnosed with gastroesophageal reflux disease 2 weeks ago returns to the office because of continued burning epigastric abdominal pain after meals. Omeprazole therapy was initiated at the time of diagnosis, but the patient reports that the pain is only partially relieved by this therapy. This is the patient’s third office visit since her diagnosis because of her symptoms. She has not had weight loss, melena, hematochezia, nausea, or vomiting. Vital signs are temperature 37.0°C (98.6°F), pulse 75/min, respirations 16/min, and blood pressure 120/80 mm Hg with no orthostatic changes. The patient appears well but anxious. Abdominal examination discloses mild epigastric tenderness to palpation but no masses. The remainder of the physical examination shows no abnormalities. Results of a serum chemistry profile and complete blood count obtained 2 weeks ago are within the reference ranges. Which of the following is the most appropriate question to ask the patient at this time?
CorrectIncorrect -
Question 22 of 50
22. Question
A 33-year-old man comes to the clinic with his mother because of a 2-month history of depressed mood that began after he lost his job in a medical records department. He also reports bodily sensations such as “electric shocks” in his arms during this time. The patient was asked to resign shortly after he informed his boss that he thought a coworker was spying on him and reporting back to the company. When the patient’s final paycheck arrived in the mail with an upside-down stamp, he thought this was a sign that he would be asked to return to his job. He left a message with his employer, which was not returned, and the patient now feels demoralized. He says he has few friends and his main social connection is with his parents. He has not experienced any auditory or visual hallucinations, decreased appetite, difficulty sleeping, or impaired concentration. The mother says the patient has been a little “different” ever since high school, but his early childhood development was normal. Medical history is unremarkable and he takes no medications. He has no family history of mental illness. Vital signs are normal. The patient is dressed in a formal button-down shirt and casual cutoff shorts. He uses words inappropriately. He has no homicidal or suicidal ideation. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 23 of 50
23. Question
A 55-year-old business executive comes to the office because of urinary incontinence. She says, “I lose control of my urine when I laugh, cough, or play tennis. I’m tired of the embarrassment. I feel like I always smell like urine.” She has five children, all of whom were delivered vaginally. She has mild hypertension for which she takes enalapril. She has had no operations. Vital signs are normal. Physical examination discloses a mild cystocele and rectocele with mild prolapse of the uterus and cervix. The cervix is normal in size and is nontender. There are no palpable adnexal masses. Which of the following is the most appropriate initial management?
CorrectIncorrect -
Question 24 of 50
24. Question
A 26-year-old man comes to the emergency department because of a constant, painful erection for the past 4 hours. He has a psychotic disorder well controlled with olanzapine and sleeping difficulties treated with trazodone. BMI is 22 kg/m2. Pulse is 110/min; remaining vital signs are normal. Physical examination shows no other abnormalities. An intracavernosal injection of a drug is administered and results in immediate flaccidity of the penis. This patient is at increased risk for which of the following conditions as a result of this treatment?
CorrectIncorrect -
Question 25 of 50
25. Question
The following vignette applies to the next 2 items.
A 20-year-old college student comes to the student health center because, she states, “I’ve had vaginal itching and a funny discharge for about 2 weeks. The cream I got from the drug store doesn’t help.” She is sexually active with only one partner, and she uses an oral contraceptive pill for birth control. She denies any previous vaginal symptoms or genital infections. Her last menstrual period was 10 days ago and was normal.
Item 1 of 2
At this time it is also most important to inquire about which of the following?
CorrectIncorrect -
Question 26 of 50
26. Question
Item 2 of 2
Which of the following physical findings would indicate a need to treat both the patient and her partner?
CorrectIncorrect -
Question 27 of 50
27. Question
A 34-year-old registered nurse who works in the coronary care unit of the hospital comes to the office for a periodic health evaluation. She says she would like to stop taking her contraceptive pill so that she can become pregnant. In addition to recommending a daily dose of folic acid, you obtain a test of rubella immune status. Results show that she is not immune to rubella. The most appropriate step at this time is to recommend that she receive the rubella vaccination and do which of the following?
CorrectIncorrect -
Question 28 of 50
28. Question
An 18-year-old man comes to the office because of a 2-year history of excessive sweating of his palms. He says, “My palms are always damp and it’s becoming a real embarrassment.” He has tried applying over-the-counter underarm antiperspirants to his hands without improvement. Medical history is unremarkable and the patient takes no medications. Vital signs are normal. His palms are damp with perspiration. The remainder of the physical examination discloses no abnormalities. Which of the following is the most appropriate initial treatment for this patient?
CorrectIncorrect -
Question 29 of 50
29. Question
A 17-year-old primigravid woman at 34 weeks’ gestation is brought to the emergency department by her parents 25 minutes after a generalized tonic-clonic seizure that lasted approximately 2 minutes. She has no history of seizures and medical history is otherwise unremarkable. Her prenatal course has been uncomplicated. Medications include a daily prenatal vitamin. The patient is alert and fully oriented. Vital signs are temperature 36.7°C (98.0°F), pulse 76/min, respirations 16/min, and blood pressure 155/90 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 99%. Fetal heart rate is 134/min and reactive. Fetal ultrasonography confirms gestational size with normal fluid; the fetus is in breech presentation. Results of laboratory studies are shown:
Blood
Urine
Hematocrit
45%
Protein
2+
Hemoglobin
14.0 g/dL
Platelet count
155,000/mm3
Results of liver function tests are within the reference ranges. Which of the following is the most appropriate pharmacotherapy?
CorrectIncorrect -
Question 30 of 50
30. Question
A 2-year-old girl is brought to the office by her mother because of a 1-day history of staggering and frequent stumbling while walking. The mother reports that the child has had no other changes in behavior, no exposure to toxins at home or to anyone who has been ill, and has not recently received any vaccines. She had spent the day with her grandmother at the grandmother’s home prior to the development of her symptoms. Vaccinations are up-to-date. Growth and development have been normal. The child is at the 50th percentile for height and weight. She appears happy. Vital signs are normal. Pupils are equal, round, and slowly reactive to light and accommodation. All other cranial nerves are intact. Gait is wide-based and the child needs support to walk. She is able to sit up with support but lists to either side when sitting independently. Which of the following is the most appropriate initial step in management?
CorrectIncorrect -
Question 31 of 50
31. Question
A 55-year-old African American man with a 5-year history of type 2 diabetes mellitus comes to the office for a routine follow-up examination. Medical history is also significant for hypercholesterolemia and benign prostatic hyperplasia. Medications include metformin, 500 mg three times daily; atorvastatin, 20 mg daily; enalapril, 40 mg daily; and finasteride. The patient does not smoke cigarettes or drink alcoholic beverages. He is 175 cm (5 ft 9 in) tall and weighs 100 kg (220 lb); BMI is 33 kg/m2. His blood pressure measurements at his past two office visits were 132/85 mm Hg and 130/86 mm Hg, respectively. Today, vital signs are temperature 37.0°C (98.6°F), pulse 88/min, respirations 20/min, and blood pressure 132/88 mm Hg. Physical examination discloses velvety brown discoloration of the axillae. Hemoglobin A1c obtained 3 days ago was 6.4%. Results of fasting laboratory studies obtained in preparation for today’s visit are shown:
Serum
Urine
Cholesterol
Specific gravity
1.029 (N=1.003–1.029)
Total
139 mg/dL
Protein
Negative
HDL
42 mg/dL
RBC
0–1/hpf
LDL
69 mg/dL
WBC
0–1/hpf
Triglycerides
140 mg/dL
Urea nitrogen
12 mg/dL
Creatinine
1.0 mg/dL
Na+
136 mEq/L
K+
4.2 mEq/L
Cl−
100 mEq/L
HCO3−
26 mEq/L
Glucose
110 mg/dL
Which of the following is the most critical factor in formulating a management plan for this patient?
CorrectIncorrect -
Question 32 of 50
32. Question

A 13-year-old boy comes to the emergency department because of persistently itchy, red blotches over his torso and extremities that developed immediately after he finished eating lunch 10 minutes ago at a local restaurant. His lunch consisted of a sandwich and a soda. He has not had any swelling of his lips or difficulty breathing. He has not had similar episodes in the past and has eaten at the same restaurant on previous occasions with no ill effects. Medical history is unremarkable and the patient takes no medications. Vaccinations are up-to-date. BMI is at the 40th percentile. The patient appears uncomfortable. Vital signs are normal. Physical examination discloses generalized skin lesions as shown in the photograph. Which of the following is the most appropriate conclusion about this patient’s condition?
CorrectIncorrect -
Question 33 of 50
33. Question
A 56-year-old man comes to the office for a routine 3-month follow-up examination for type 2 diabetes mellitus, peripheral vascular disease, hypertension, and hyperlipidemia. The patient says that he has gained approximately 9 kg (20 lb) during the past 6 months. He attributes his weight gain to his sedentary job as a night security guard. Medical history also is remarkable for bilateral femoropopliteal bypass grafting 3 years ago. Current medications include clopidogrel, enalapril, amlodipine, metformin, furosemide, and simvastatin. His father died of a myocardial infarction at age 62 years. The patient’s mother has hypertension, type 2 diabetes mellitus, and Alzheimer disease. The patient is 178 cm (5 ft 10 in) tall and weighs 113 kg (250 lb); BMI is 36 kg/m2. Vital signs are temperature 37.0°C (98.6°F), pulse 80/min, respirations 14/min, and blood pressure 150/80 mm Hg. Examination of the skin discloses slightly darkened pigmentation of the ankles and distal lower extremities. Cardiac examination discloses a grade 2/6 systolic ejection murmur heard best at the right second intercostal space and radiating to the carotid arteries. Liver span measures approximately 14 cm by percussion, and palpation of the liver edge discloses no tenderness. Pedal pulses are decreased bilaterally. The patient should be informed that he is at greatest risk for which of the following conditions?
CorrectIncorrect -
Question 34 of 50
34. Question
A 55-year-old man, who has lived alone in a cabin in the woods for the past 6 years, is brought to the emergency department by his daughter 3 hours after a forest ranger found him in bed having protracted episodes of vomiting. On the patient’s arrival at the emergency department, vital signs are temperature 37.8°C (100.0°F), pulse 100/min, respirations 28/min, and blood pressure 90/60 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 97%. The patient is lethargic and cachectic. Skin turgor is decreased and oral mucosa is dry. He is resuscitated and arrangements are made to admit him to the hospital. Results of serum laboratory studies in this patient are most likely to show which of the following?
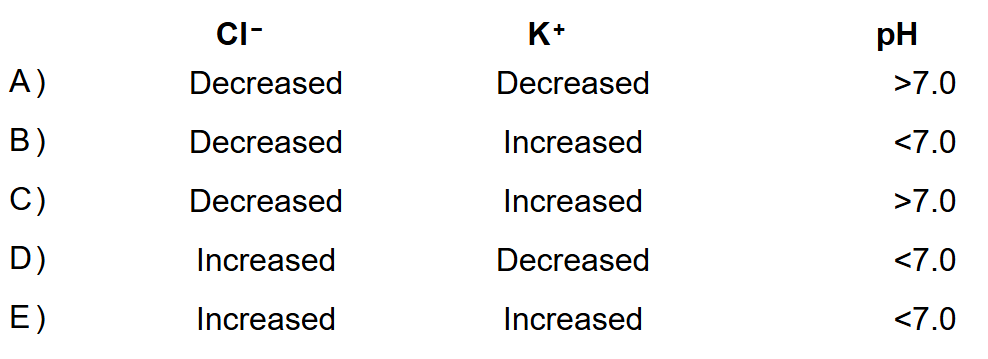 CorrectIncorrect
CorrectIncorrect -
Question 35 of 50
35. Question
A 9-year-old boy is admitted to the hospital because of a 24-hour history of progressive headache, neck stiffness, and fever. Five days ago, he had an upper respiratory tract illness and two episodes of diarrhea that have since resolved. Medical history is otherwise unremarkable and the child takes no medications. He lives with his parents and two younger siblings, and is a third grader at a local elementary school. None of his family members or classmates have had similar symptoms. The patient is in moderate distress. Vital signs are temperature 37.8°C (100.0°F), pulse 106/min, respirations 16/min, and blood pressure 100/60 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. Physical examination discloses mild nuchal rigidity but no tremors. Gram stain of cerebrospinal fluid shows gram-negative diplococci. Culture results are not yet available. Antibiotic therapy is initiated. Which of the following is the most appropriate intervention at this time?
CorrectIncorrect -
Question 36 of 50
36. Question
An 88-year-old Portuguese woman is brought to the emergency department by her daughter because of a 2-day history of abdominal bloating and yellowing of the skin that they noticed today. The patient has not had abdominal pain and has continued to eat meals regularly. Medical history is unremarkable and she takes no medications. She does not smoke cigarettes or drink alcoholic beverages. On arrival at the emergency department, the patient appears jaundiced. Vital signs are temperature 37.2°C (99.0°F), pulse 92/min, respirations 18/min, and blood pressure 110/74 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 92%. Abdominal examination discloses distention and diffuse tenderness to deep palpation but no guarding. Which of the following is the most appropriate diagnostic study at this time?
CorrectIncorrect -
Question 37 of 50
37. Question
A 52-year-old woman is brought to the emergency department by ambulance because of an 8-hour history of worsening back pain, bowel and bladder incontinence, and weakness in both legs. The patient reports no recent trauma, but her medical history is significant for herniations of the L3, L4, and L5 discs that were diagnosed 2 years ago and treated with analgesics and physical therapy. Medications include nonsteroidal anti-inflammatory drugs and oral narcotics as needed for pain. The patient appears mildly uncomfortable. BMI is 33 kg/m2. Vital signs are normal. Physical examination discloses tenderness over L3, L4, and L5 at the midline. There is weakness on dorsiflexion and plantar flexion of both feet. Achilles deep tendon reflexes are decreased bilaterally. Sensation at the perirectal area is decreased, as is rectal tone. Which of the following is the priority in management?
CorrectIncorrect -
Question 38 of 50
38. Question
A 52-year-old man is brought to the emergency department by his wife because of a 2-hour history of chest pain. Medical history is significant for asthma and visual impairment secondary to Leber congenital amaurosis. Outpatient medications include inhaled albuterol and fluticasone. On arrival, vital signs are temperature 36.1°C (97.0°F), pulse 92/min, respirations 18/min, and blood pressure 136/84 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 94%. Cardiopulmonary examination discloses no abnormalities. ECG shows 2-mm ST-segment elevations in the anterior leads. Preparations are made to take the patient to the cardiac catheterization laboratory. Which of the following is the most appropriate action regarding informed consent prior to proceeding with this patient’s cardiac catheterization?
CorrectIncorrect -
Question 39 of 50
39. Question
A 68-year-old man is brought to the emergency department by his family because of the sudden onset 90 minutes ago of right-sided weakness and garbled speech. The patient has no history of neurologic disease. Medical history is significant for hypercholesterolemia, managed with atorvastatin, and a cholecystectomy 15 years ago. He takes no other medications. Vital signs are temperature 37.0°C (98.6°F), pulse 90/min, respirations 16/min, and blood pressure 155/98 mm Hg. Pulse oximetry on 40% oxygen via face mask shows an oxygen saturation of 100%. The patient is alert and responsive but aphasic. There is a right facial droop. Cardiac examination discloses a regular rhythm without murmur. There is a left carotid bruit. Peripheral pulses are normal bilaterally. Muscle strength, deep tendon reflexes, and sensation to pinprick in the upper and lower extremities are intact on the left and absent on the right. CT scan of the head shows no hemorrhage. The most appropriate pharmacotherapy to initiate for this patient is likely to improve his outcome through which of the following mechanisms?
CorrectIncorrect -
Question 40 of 50
40. Question
A 70-year-old man is admitted to the hospital for a total hip replacement operation. Two days after the procedure he has dyspnea, and he is in acute distress with right-sided chest pain. Medical history is remarkable for ureteral calculi and emphysema. Vital signs are temperature 37.2°C (99.0°F), pulse 100/min, respirations 32/min, and blood pressure 100/70 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 80%. Auscultation of the chest discloses clear lungs, regular rhythm, and a grade 2/6 systolic murmur audible at the upper right sternal border. Results of serum laboratory studies are shown:
Urea nitrogen
19 mg/dL
Creatinine
1.2 mg/dL
Administration of intranasal oxygen at 2 L/min produces the following changes:
Room Air
Intranasal Oxygen
Po2
49 mm Hg
55 mm Hg
Pco2
52 mm Hg
54 mm Hg
pH
7.34
7.36
Respirations
28/min
26/min
The patient remains dyspneic despite receiving oxygen therapy. Chest x-ray shows no abnormalities. Which of the following is the most appropriate diagnostic study?
CorrectIncorrect -
Question 41 of 50
41. Question

A 4-year-old girl is brought to the office by her parents for a well-child visit. Medical history is unremarkable. The patient’s only medication is a daily multivitamin. The child appears happy and is drinking milk from a bottle. She is at the 50th percentile for length, weight, and head circumference. Vaccinations are up-to-date. Vital signs are normal. Physical examination discloses the oral findings shown. The remainder of the examination discloses no abnormalities. Which of the following is the most likely causal agent for this patient’s condition?
CorrectIncorrect -
Question 42 of 50
42. Question
A 68-year-old woman returns to the clinic to discuss results of a DEXA scan obtained 1 week ago. Medical history is unremarkable and she takes no medications. She does not smoke cigarettes. BMI is 27 kg/m2. Temperature is 36.7°C (98.0°F), pulse is 80/min, respirations are 12/min, and blood pressure is 120/75 mm Hg. Physical examination 1 week ago showed no abnormalities. Results of DEXA scan show a T-score of −1.8. Fracture risk assessment score is 10.6% for a major osteoporotic fracture and 1.65% for a hip fracture. Which of the following is the most appropriate next step in management?
CorrectIncorrect -
Question 43 of 50
43. Question
A 23-year-old man is brought to the emergency department by his girlfriend 4 hours after she found him on the floor of their apartment crying. There was an empty bottle of acetaminophen near him. Medical history is remarkable for major depressive disorder diagnosed 1 year ago. His only prescribed medication is citalopram. Vital signs are within normal limits. Physical examination discloses no abnormalities. Serum acetaminophen concentration is 40 mg/L. Results of a complete blood count and serum creatinine, sodium, and glucose concentrations are within the reference ranges. Serum and urine toxicology screening is negative. Results of liver function tests are within the reference ranges. ECG shows no abnormalities. Two hours later, serum acetaminophen concentration is 20 mg/L. The patient says he was not trying to hurt himself and that “this is just a misunderstanding.” He demands that he be released immediately. Which of the following is the most appropriate next step in management?
CorrectIncorrect -
Question 44 of 50
44. Question
A 55-year-old man comes to the emergency department because of a 3-week history of worsening shortness of breath and cough productive of bloody sputum. The patient initially noticed shortness of breath when lifting heavy boxes at work, but he is now short of breath at rest. Medical history is unremarkable and he takes no medications. The patient has smoked one pack of cigarettes daily for the past 40 years. Vital signs are temperature 37.4°C (99.3°F), pulse 105/min, respirations 30/min, and blood pressure 148/75 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 80%. After initiation of oxygen therapy at 4 L/min via nasal cannula, oxygen saturation improves to 92%. Physical examination discloses an enlarged right supraclavicular lymph node. Auscultation of the lungs discloses inspiratory and expiratory wheezes on the right. Chest x-ray shows a spiculated 3 × 3-cm mass in the right hilum. Which of the following is the most appropriate next step in establishing the diagnosis?
CorrectIncorrect -
Question 45 of 50
45. Question
A 69-year-old man with metastatic prostate cancer is admitted to the hospital because of a 1-week history of increasingly severe pain in the spine and all extremities. He rates his pain as a 10 on a 10-point scale. He received hormone therapy for 2 years and chemotherapy during the past year. His only medication is morphine, which provides insufficient relief of his pain. The patient appears to be in distress. Vital signs are temperature 37.0°C (98.6°F), pulse 112/min, respirations 28/min, and blood pressure 145/88 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 99%. On examination, he is cachectic and grimaces with any movement in his bed. The remainder of the examination shows no abnormalities. Radionuclide bone scan shows extensive metastases with multiple new areas of distribution. The patient requests additional pain medication. Which of the following is the most appropriate next step in management?
CorrectIncorrect -
Question 46 of 50
46. Question
A 3-year-old boy is brought to the emergency department by his father because of a 2-day history of severe right ankle pain. He cannot bear weight on his right leg. Medical history is remarkable for two episodes of otitis media at ages 1 year and 18 months, respectively. He currently receives no medications. He attends day care. He is at the 30th percentile for height and 25th percentile for weight; BMI is at the 26th percentile. Temperature is 38.5°C (101.3°F), pulse is 100/min, respirations are 16/min, and blood pressure is 120/80 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. Examination of the right lower extremity discloses warmth and swelling of the right ankle with severe pain on flexion and extension. Aspiration of the joint yields purulent synovial fluid. Gram stain of the fluid shows gram-positive cocci in clusters and many segmented neutrophils. Nucleic acid amplification test of the fluid discloses Staphylococcus species and presence of the mecA gene. The most appropriate pharmacotherapy for this patient targets which of the following?
CorrectIncorrect -
Question 47 of 50
47. Question
Investigators conduct a randomized, placebo-controlled trial to evaluate a new medication for the treatment of systolic dysfunction heart failure and determine if the medication would decrease mortality rate. A total of 3000 patients are needed, using a sample size calculation that incorporated an expected baseline mortality rate of 20% for the placebo group and 15% for the intervention group. The trial will last 3 years, and interim safety monitoring will occur annually. Data from the interim analyses after years 1 and 2 are shown:
Relative Risk
Treatment Group
Mortality Rate, %
(95% Confidence Interval)
P-value
Year 1
Intervention
23
1.15 (0.95 to 1.30)
.09
Placebo
20
—
Year 2
Intervention
22
1.10 (0.98 to 1.21)
.07
Placebo
20
—
Safety monitors calculate that for the new medication to demonstrate benefit by the end of the study, the remaining recruited patients in the intervention group would need to have a mortality rate of less than 7%. Based on this information, which of the following is the most appropriate recommendation by the safety monitoring board to the investigators regarding this trial?
CorrectIncorrect -
Question 48 of 50
48. Question
A 60-year-old man with a history of alcohol use disorder comes to the emergency department because of severe epigastric pain and nausea. During the past 4 years, he has had three episodes of alcoholic pancreatitis and says that these symptoms feel similar to those episodes. He has not consumed alcohol in 3 years. He also has hypertension and hyperlipidemia. His medications are amlodipine and atorvastatin. He is diaphoretic and sitting forward clutching his abdomen. Vital signs are temperature 36.1°C (97.0°F), pulse 100/min, respirations 14/min, and blood pressure 150/90 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 98%. Abdominal examination discloses upper abdominal tenderness to palpation. Measurements of liver and pancreatic enzyme activities are within the reference ranges. While waiting to be admitted, the patient’s systolic blood pressure decreases to 70 mm Hg and is palpable. Administration of 0.9% saline is begun. An ECG shows findings consistent with an inferior wall myocardial infarction with right ventricular infarct. Which of the following is the most likely explanation for the diagnostic error made by the physician?
CorrectIncorrect -
Question 49 of 50
49. Question

A 71-year-old man comes to the office with his wife for an initial visit because of a non-itchy, painless spot on the patient’s back that the patient thinks has been present for several years. His wife notes that the spot has enlarged and become darker during the past several months. The patient’s medical history is unremarkable and he takes no medications. Vital signs are normal. Physical examination discloses no adenopathy. Examination of the patient’s back discloses the lesion shown in the photograph. The remainder of the physical examination discloses no abnormalities. Which of the following is the most appropriate next step in management?
CorrectIncorrect -
Question 50 of 50
50. Question
A 65-year-old man comes to the clinic because of a 2-year history of progressively worsening shortness of breath. He now becomes short of breath and needs to stop and rest after walking approximately 100 feet. He also has had an occasional cough, which is intermittently productive of clear sputum in the morning. He has not had shortness of breath at rest or chest pain. Medical history is remarkable for hypertension and his only medication is lisinopril. He smoked one pack of cigarettes daily for 40 years but quit 8 years ago. Temperature is 37.0°C (98.6°F), pulse is 78/min and regular, respirations are 14/min, and blood pressure is 122/66 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96% at rest; after the patient walks 50 feet, he appears mildly short of breath and oxygen saturation decreases to 93%. Auscultation of the lungs discloses mildly decreased breath sounds bilaterally with no wheezes, rhonchi, or crackles. There is no clubbing of the fingers or cyanosis. The remainder of the physical examination discloses no abnormalities. Results of laboratory studies are shown:
Serum
Blood
Urea nitrogen
8 mg/dL
Hematocrit
47%
Creatinine
0.6 mg/dL
Hemoglobin
16.2 g/dL
Chest x-ray shows no opacities. Spirometry discloses an FEV1 of 78% of predicted and an FEV1/FVC ratio of 66%. In addition to inhaled albuterol therapy, which of the following is most appropriate management at this time?
CorrectIncorrect